An IV slowly drips out the passage of time as a patient lies nearby, sick of waiting. Like others in need of a transplant, she can do nothing but wait, her spot just one of thousands on a waitlist that, according to the United Network for Organ Sharing, grows every 10 minutes. But instead of being put on a waitlist, what if she could just have a new kidney printed? The field of regenerative medicine, which aims to develop techniques to create tissues and organs for patients, may someday make this a reality, and a necessary one at that; as people live longer, there is a growing need for transplantable organs that the current system cannot handle.
Inspired by this growing need, Anthony Atala, MD, the Director of the Wake Forest Institute for Regenerative Medicine, and his team have worked on refining the use of inkjet printers and 3D printers to create tissues and organs. In 2011, Dr. Atala presented his work in regenerative medicine at a TED Talk, and since then he and his team have made even more progress towards a future where we can print out the organs we need. Here, you’ll find the full interview from my opportunity to speak with Dr. Atala about his research, past and present, how far he’s come since that TED Talk, and the medical applications of 3D printing.
If you could start by telling me a little bit about yourself and how you ended up in the field of regenerative medicine.
I’m actually a surgeon, by training, but I also do research, so I do both; I’m both a clinician and researcher. Those kind of evolved into the field of regenerative medicine, which took 25 years, (three in its infancy) before the term was actually coined. The goal really, was trying to create tissues and organs for patients. The whole impetus for that was the need for the patients, you know; what is needed for the patients? That’s a condition, and looking at that need, for example, motivated me, motivated our work, to be directed towards the area of regenerative medicine. And that’s where we create tissues and organs for patients with disease or injury.
Was that also motivated by the shortage of organs and tissues that the organ donor system has? From what I can tell there are far more patients that need organs than there are organs available.
Absolutely, and it’s a growing need. In a ten-year period, the actual number of patients [waiting for a transplant] on the waitlist doubled. But in that same time period, the actual number of transplants barely went up about only 1%. We’re aging, we’re living longer, we’re aging better, and as a result more organs fail as we age, so the need for organs has really increased.
Explain to me your technique for 3D-Printing organs. Did you come up with it, or was there a history of this technique that already existed that you worked on or perfected?
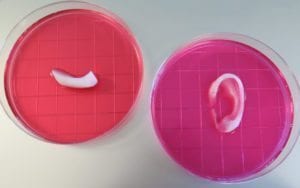
We actually got our start by creating tissues by hand, and that’s important to realize. Basically, we really started out by trying to create tissues for patients. The concept there is to take a very small piece of tissue from the patient, less than half the size of a postage stamp. We then are able to expand the cells in that tissue. Once we have enough cells to create the tissue or the organ, usually after about 4-6 weeks, we constitute the whole thing by hand. We created the tissue by hand by basically seeding the cells on these three-dimensional scaffolds. Then we’d put that in an oven-like device, very much like baking a layer-cake if you will. In that oven-like device, an incubator, we let it cook for a while or, if you will, mature. And then you’d put it back into the patient.
That’s what we started doing over 25 years ago, that’s the technology we started working on. And then, once we were able to apply that to patients in several applications, once we started to do that, we then decided that, you know, it was fine to make these things by hand if you were doing a small number of patients in clinical trials. But if you really wanted to scale up the technology…You really needed to automate the process, and that’s when we started thinking about using your typical desktop inkjet printer, which is what we started to use fourteen years ago. We started using your typical desktop inkjet printer that we modified, so that instead of printing ink, we would print cells, with a gel. We modified these printers…so every time the print-head would go through, the elevator would lower itself. Basically, picture printing on a piece of paper over and over and over again, in the same region, simply printing one layer at a time which creates three-dimensional structures. That’s how we got our start with it.
Then we realized that it was fine to print these cells, but they really didn’t have the structural integrity that was required for a tissue to be implanted. So we started to build our own printers. For the last 11 years or so we started building our own printers. We’ve come up with technologies and printing systems with printers that we built that are strictly limited to the creation of tissues and organs.
Was there a “Eureka!” moment when you decided to use inkjet printers, or was it a natural progression as you realized that hand-making tissues was far too inefficient to be viable?
It was a gradual process. The technology for printing has, of course, been around for several decades. Really, it’s how can you actually use these technologies to apply it to really scale up what we were doing by hand. Obviously there’s nothing that’s magical about a printer, right, because you have to program the printer to do what you need it to do [laughs]. So in other words, we still have to make sure that the cells are the right cells, we still have to make sure we put them together in the right way.
You have to learn how to make it by hand before you can automate the process. You have to have all the complexity of creating a tissue managed, in terms of biology of the cells, the molecular biology, the genetics, the biomaterials sciences, the physiology, the pharmacology, the biochemistry. All of that has to be worked out in creating this tissue before you can actually say “How are you going to scale it up? How are we going to automate the process?”
So, in order to have even come this point at all, where you decided to use printers, it’s really important to understand how it works from a layer-by-layer standpoint?
Yes.
Earlier you mentioned some scaffolding; how does that work? Is there more to the process of 3D-printing an organ than just “layer-by-layer?”
So, these printers that we have developed, they have four features that allow us to create these structures. The first feature…you need precision. You need to lay down the cells exactly where they need to be. We use some very small nozzles, that go all the way down to 1-2 microns, which is about 1/80th the diameter of a single human hair. They are very, very small nozzles.
The second feature is that we need to make sure that the cells don’t get damaged in the process, so we need to make sure that they go through the nozzle as a liquid, but then also we need to make sure that they retain their shape once we print the structure, so they don’t just splatter everywhere. The way that we do that is by making sure that the cells go down as a liquid, but once they leave the nozzle and hit the surface, they need to be more like gelatin, where they keep their shape. And then, in the next tens of minutes, it needs to harden like a gummy bear. It’s a conversion of these materials that we use that we can make these materials go from liquid, to a gelatin, to a gummy bear consistency within a defined period of time. And the way that we do that…we actually create bio-inks that have hard and soft components to them. Just like when you were building Lincoln Logs, but just picture every other log being softer. That’s the way we do it. Therefore, the rigid structures are able to maintain their structural integrity with what you’re trying to do while the soft structures are nourishing the cells.
The third thing is to make sure that you’re able to make sure that nutrition gets to the central portion of that tissue. It’s very important, since nutrition needs to get to all the cells in order for them to survive. The main thing there, is to make sure that we have the ability to have these micro-channels that allow nutrition to go through the central portion of the construct, and these micro-channels basically act like a highway that bring nutrition into the central portion of the core, allowing these tissues to survive. That’s really the other big parameter for it.
Finally, the fourth one is to make sure that we can use CAD [computer aided drafting] software printing programs, so that we can match to the patient’s needs. So we do an x-ray of the patient, and we are able to transfer that information from patient to the printer, so we can create the size that will fit the patient, you know, making it personalized matter.
How much trial and error did you have to go through before your idea was realized? In other words, what was the process in figuring out these four necessary qualities of your 3D printing material?
A LOT of trial and error. All these things have to be put through a lot of trial and error, making these things over the years. And in an integrated manner, right? So, it’s not just having one feature, but all of them working together. Really, that’s why it took eleven years’ worth of work. We just published that work in March of this year in Nature Biotechnology.
Would you call yourself a pioneer in this field with this technique? I know it’s been around for a while, but would you consider yourself one of the first people to start using it and refining it at its current level?
You know what, that’s not for me to say. We work hard at what we do, obviously, but we’re always standing on the shoulders of giants that came before us, and that’s true for any science that you do.
It seems like you have made significant progress in the last five years since your TED Talk. How different are the results now than they were five years ago?
The main difference is that we could create these tissues, but they could not be implanted surgically. We could create these tissues and they would remain viable in vitro, but now we can do so and also implant them surgically, where they actually, pre-clinically in research studies…can get good vascularity and good innervation inside the body.

And just to be clear, when we’re talking about actually “putting them in patients,” that includes organs? Or is it still just tissue?
There are different levels of complexities in terms of tissues and organs, with flat structures, like skin being the least complex; tubular structures, like blood vessels, being the second level of complexity; hollow, non-tubular organs being the third level of complexity; and solid organs, like the heart or the liver, being the fourth level of complexity…It goes from least complex to most complex, and up to this point, we’ve been able to implant the first three types of organs into patients. We have not yet implanted a solid organ, at this point. That’s really a lot of the work that we’re doing right now to make that possible; in a patient that is.
So you can actually print a stomach or a bladder for a patient based on an X-ray, and then implant that in them and it will function and integrate with their body?
Yeah, well, not printed so far; but we’ve made these by hand and we’ve put them into patients.
And they work?
Right, correct.
That’s incredible.
Now, the key is “how do we scale up the technology to make sure that we have more?” Now that we’ve made them by hand, and now that we have them in patients, and they work, how can we automate the process? And also, how can we tackle the new tissues as well that we have not yet put into patients?
Based on all of that, where do you see this technology in the next five or ten years?
I would say that when it comes to these technologies, when it comes to putting them in patients, you can never rush it, you know? Regardless of technology, you always have to prove safety, and you have to go through that process. Yes, we are definitely more advanced than we were just five years ago, and ten years ago. But it’s really hard to predict where we will be in the future because it involves patients, and when it comes to patients the number one directive is safety.
In our lifetime, do you think that creating and implanting all types of organs is an achievable goal? Or are there limitations?
I think to actually take these technologies that we actually created by hand and now switch that to bio-printing…I think that’s a very doable goal.