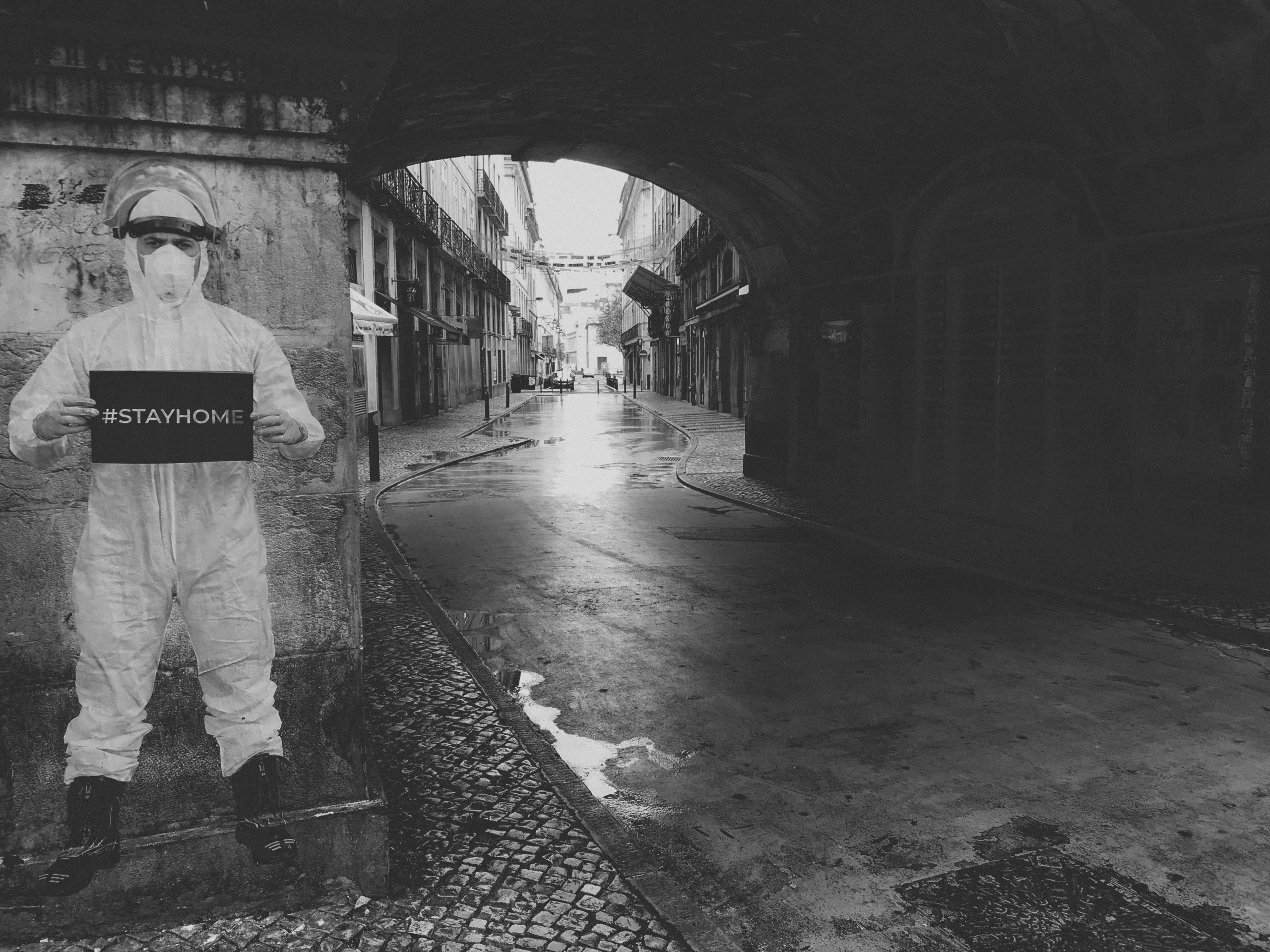
The global war against the coronavirus pandemic continues to wage on while researchers and medical experts seek to find a cure for COVID-19 symptoms. While many believe this is here to stay for an indefinite period, others feel that this too, shall pass.
The number of confirmed cases and death rates only seem to darken our world with over 400,000 confirmed cases in New York, the death toll is now over 31,000, with over 233,000 confirmed cases in Florida, the death toll is now over 4,000, and with over 250,000 confirmed cases in Texas, the death toll is now over 3,000.
And here we are in July 2020 where you can simply add those statistics and drive to find a cure for COVID-19 to our to-do list in the war on cancer and other diseases that still have not seen a cure.
With Florida continuing to make headlines by the day, most recently with one family facing federal charges after allegedly marketing a toxic bleach solution as a cure for multiple ailments, including COVID-19, the timing for our society to come together to help find a cure is essential.
And no, we’re not kidding. The Florida family (Mark Grennon and his three sons) were charged Wednesday with conspiracy to defraud the United States, conspiracy to violate the Federal Food, Drug and Cosmetic Act, and criminal contempt, according to the Department of Justice.
As for the Florida community, one Tampa business has been conducting the first-in-human clinical study for cutaneous melanoma. Morphogenesis, a clinical-stage company developing novel cell and gene therapies has been making headlines after receiving FDA approval to expand its human clinical trials into two more types of cancer: Merkel cell carcinoma (MCC) and cutaneous squamous cell carcinoma (cSCC).
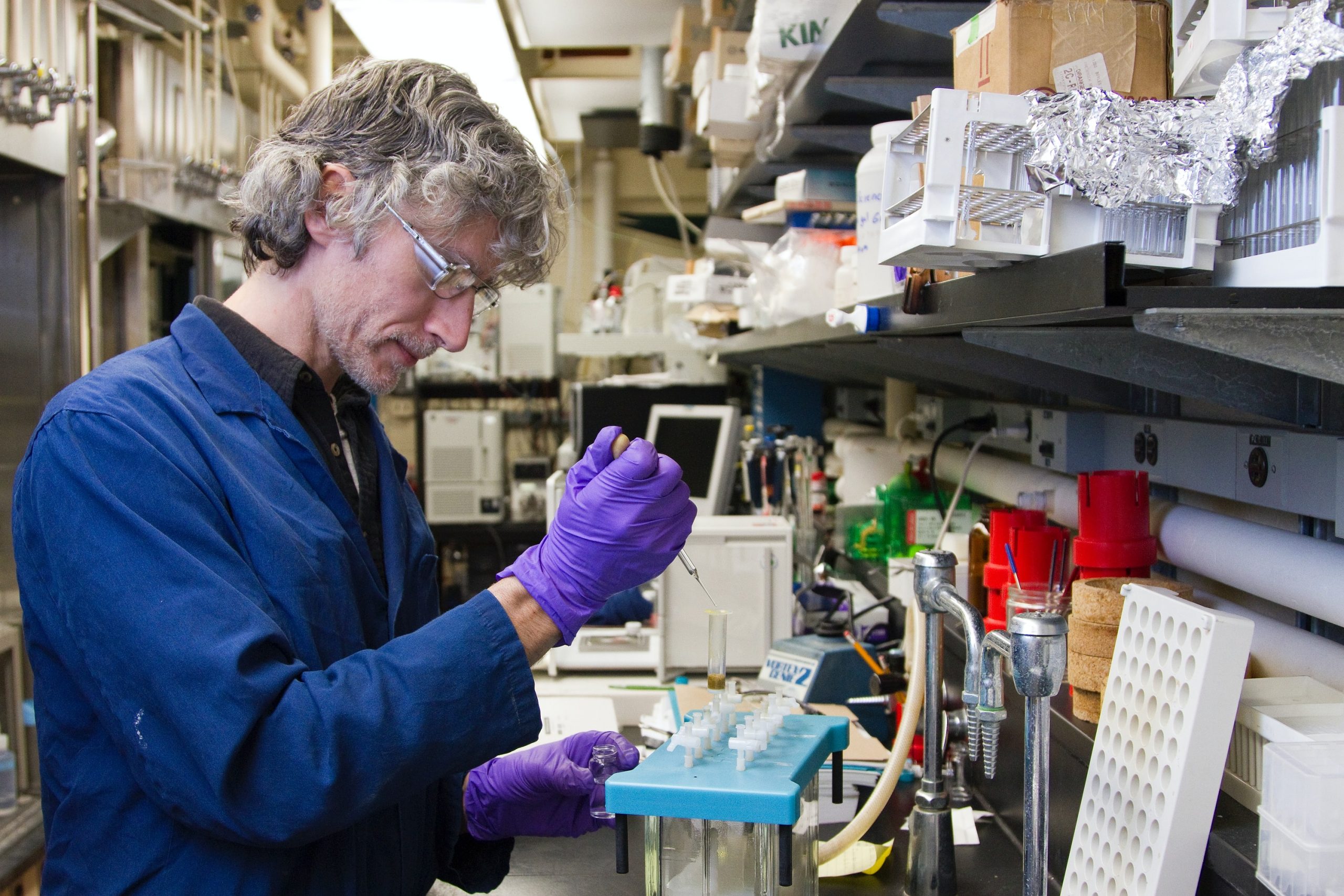
Using its ImmuneFx (IFx) cancer vaccine technology that initiates the power of the immune system on the destruction of tumor cells, Morphogenesis of Tampa will focus its newly FDA approved trials on understanding these two new cancers, which follows in the footsteps of successful human trials on cutaneous melanoma, conducted in cooperation with Moffitt Cancer Center in 2019.
Other MCC and cSCC clinical trial sites across the country include the University of Southern California, the University of Utah, the University of Colorado, and the Dana Farber / Harvard Cancer Center. So why so many trial sites?
Well, according to Morphogenesis CEO Dr. Patricia Lawman, clinical trials need patients, which to qualify, requires an individual having been diagnosed with advanced Merkel or cutaneous squamous cell carcinoma, and having failed or refused other therapies.
As a cell and gene company, the mission from the beginning was to learn from the body and use the body’s building blocks and communication systems to treat chronic disease. Morphogenesis, according to Lawman, was built to identify, isolate and proliferate stem cells and progenitor cells to treat diseases such as diabetes.
With the world united to change the way in which chronic diseases are treated by engaging the innate intelligence of the body, how do companies (on a local level) push for national change?
“The ability to genetically modify stem cells to enhance functionality is one aspect of this, but in order to perform a biological function, the stem cells must differentiate into mature cells, e.g. hematopoietic stem cells differentiate into macrophages that perform phagocytic and antigen presentation functions and T cells that kill cancer cells or virally infected cells. ‘Morphogenesis’ means the evolution of form, which connotes the change for stem cells to these functional cells capable of mitigating chronic disease.”
And what this means for our bodies, according to Lawman, is that regardless of the species, our bodies have developed systems that maintain structure and function over a long period of time. “When we need to control blood sugar, beta islet cells produce just enough insulin as needed.”
Indeed with modern technology, you would think that this is a relatively easy process to control.
“There is an exquisite feedback system that regulates this. When things go awry, our best solution has been to provide insulin through pumps that are controlled in part by constant glucose monitors. This one example of where modern technology has tried to solve a problem mimicking how the body works.
However, even providing insulin through a pump can’t do what a pancreas can. When it comes to dealing with foreign invaders, the immune system is unequaled. No drug, small molecule or compound can eliminate an invader as well as a fully functional immune system. We can kill cancer cells (while not foreign, they are still invaders) with chemo and radiation, but given the proper assurance, the immune system can eliminate the invader and do it with fewer adverse effects. Almost always, the body performs healing functions better than a synthetic drug or compound.”
The company’s recent FDA approval to move forward with stage 2 of its clinical trials is a gigantic win for the company’s mission. “The ability to expand our proof of concept studies from a single skin cancer into other, quite different skin cancers under the same Investigational New Drug (IND) is the next step in the execution of our clinical development plan.”
And that starts with Morphogenesis’ focus on “easily accessible tumors.”
“Since our therapy can be used to treat virtually any type of cancer, we wanted to start out with easily accessible tumors that could be directly injected with our plasmid DNA. The safety data collected from the cutaneous melanoma, Merkel cell carcinoma and cutaneous squamous cell carcinoma Phase 1 trials is a Segway into a Phase 2 skin cancer basket trial testing IFx-Hu2.0 as a monotherapy and in combination with a checkpoint inhibitor.”
But anytime there is discussion over stem cell research or breakthroughs in the war on cancer, of course comes naysayers and disbelievers.
One thing that Dr. Lawman has noticed is the bias within scientific circles.
“In scientific circles, there has been a bias against simple solutions, including the assumption that to get efficient transfer of genetic material you need viral vectors for all applications. These vectors are complicated to manufacture and use and pose a certain amount of risk to the patients. Plasmid DNA or mRNA, on the other hand, are much safer and are a viable alternative to viruses.
As an example, we inject our plasmid DNA directly into a patient’s tumor. We get sufficient uptake and expression of our protein to initiate an immune cascade with the effect spreading to multiple tumor antigens. The use of a viral vector in this case would be an unnecessary complication and risk.”

Now in today’s landscape with COVID-19 putting more pressure on experts to find a cure, Morphogenesis, like any company, is similarly faced with logistical challenges and supply issues.
“COVID-19 has certainly affected patient recruitment to our trials. Hopefully, ways will be developed for patients to receive treatment for their terminal diseases even if restrictions continue. Otherwise, the death rate for these patients will be much higher than COVIDs. The biggest challenge for us is the continual process of raising funds that all small biotechs face.”
As for ImmuneFx, the company’s newest vaccine, we got the exclusive.
“Beyond the Phase 2 skin cancer trial, we will be opening trials for head and neck cancer, gastric cancers, cervical cancer and colorectal cancer. The value add here is that successful trial results in multiple types of cancer will substantiate the efficacy and expand our label claims.”
But with new products and solutions, come criticism. Lawman added that the one thing that is not usually discussed in such conversations is “the importance of the safety profile of a new product.”
“Some of the new cellular immunotherapies not only come with a hefty price tag, the cost of treating the adverse side effects caused by the therapies can be as much as double the cost of the therapy itself (up to $1.5M total). Some of the newer gene therapies can have a price tag of up to $2M per treatment.
Not only can our plasmid DNA be cost effectively manufactured, it is causing minimal side effects, i.e. what we saw in hundreds of companion animals with naturally occurring cancers is being born out in human patients. Both of these cost saving factors means that ultimately, millions of people will have access to cancer treatment who otherwise would have none.”